Otoscopy is performed routinely in the hearing clinic, in virtually every appointment. It’s also a task that can be performed by clinic assistants and support staff. This blog is a fundamental review of the essentials of otoscopy and can be used as a refresher or as an aid to teaching support staff how to perform otoscopy. Let’s jump in!
What is Otoscopy?
Otoscopy is a clinical procedure used to examine the ear canal and eardrum using an otoscope.
What is an Otoscope?
Traditionally, an otoscope is a handheld device with a light source and a magnifying lens and speculum, used for visually examining the ear. Alternatives to traditional otoscopes include handheld video otoscopes and head-worn otoscopes.
How to Perform Otoscopy
- Explain the procedure to the patient and ensure that they provide consent.
- Position the patient appropriately, which usually involves them sitting upright with their head tilted toward the opposite side of the ear that is being examined.
- Ensure the otoscope is clean and in good working condition.
- Attach the appropriate size of speculum to the otoscope. The speculum is the part of the otoscope that goes into the ear canal.
- Turn on the otoscope’s light source to provide adequate illumination.
- Grasp the otoscope like a pen, either using your dominant hand or, ideally, matching the hand you use to the patient’s ear (i.e., use right hand to visualize the right ear).
- Use the other hand to gently pull the patient’s pinna upward and back (for adults) or downward and back (for children) to help straighten the ear canal.
- Carefully and gently insert the speculum end of the otoscope into the ear canal.
- Avoid applying excessive pressure or pushing too deep, as this can cause discomfort or injury.
- Direct the otoscope downward and slightly forward to follow the natural curve of the ear canal.
- Slowly advance the otoscope while observing the ear canal and eardrum.
- Look for any signs of abnormalities, such as earwax buildup, inflammation, infection, foreign objects, or perforation of the eardrum.
- Take note of the eardrum’s color, position, and any visible landmarks.
- After completing the examination, gently withdraw the otoscope from the ear canal.
- Record your findings, including any abnormalities or observations made during otoscopy.
- Discard the speculum and clean the otoscope with an appropriate disinfectant to prevent cross-contamination.
Normal Otoscopic Findings
For clinic support staff performing otoscopy, you are usually looking to identify whether the ear is clear of otologic red flags or abnormalities prior to booking or prioritizing an appointment. So, what is a normal otoscopic result?
The appearance of the ear canal, using magnification and illumination, should reveal healthy tissues and an unobstructed view down the canal to the tympanic membrane. The colour of the skin in the canal should be similar to the individual’s skin colour with the tympanic membrane appearing either a light gray or pearly white. There should not be an appearance of bulging at the tympanic membrane.
Let’s look at four examples of normal otoscopy:
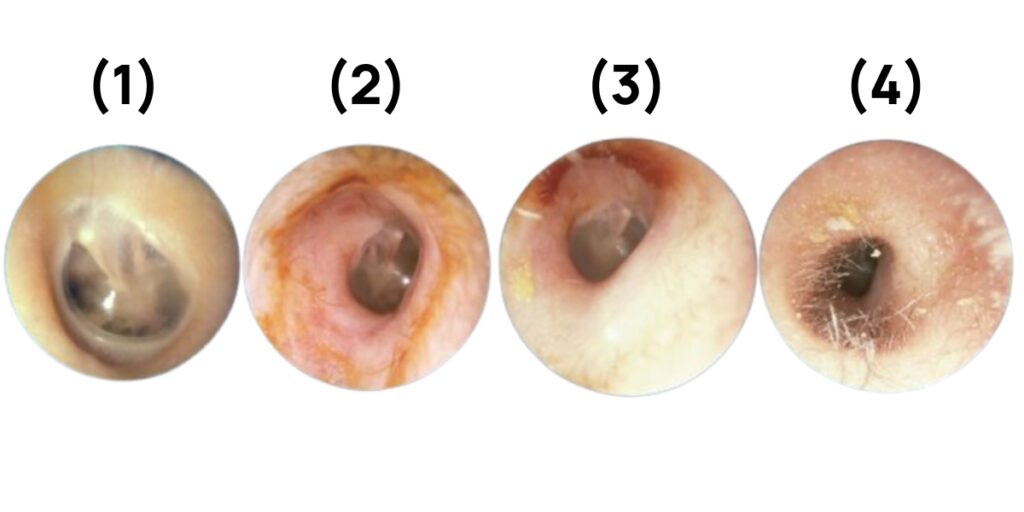
- This is a normal tympanic membrane, featuring the cone of light, which is a reflection from the light of the otoscope that can be seen here at 7 o’clock. The middle ear bones are visible through the translucent tympanic membrane.
- In the next picture, we see the isthmus, which is the transition from the cartilaginous to bony sections of the external ear canal. Notice that in the cartilaginous portion of the canal, there is some cerumen and hair. In the bony section, you do not see either of these and the skin looks visibly thinner.
- Next, we take a deeper look into the canal at the bony section, again noticing no hair and smooth thin skin, and the second bend of the canal is visible in this picture.
- Finally, we look at some hair in the cartilaginous portion. You can see some cerumen on the hair, and you can also see the two bends in the canal here. You cannot clearly see the tympanic membrane in this picture as the otoscope is placed quite shallowly at the opening of the auditory meatus.
Otoscopy is a skill that gets developed with practice. If you work as a clinic support staff what would like to begin performing otoscopy, consider using a video otoscope so that you can take photos and discuss the findings with your hearing care professionals to develop your skill and expand your knowledge.
To learn more about common abnormal conditions of the external ear, please head over to our blog here.
Thanks for reading! If you found this blog useful, please share it.





